
Paths to Practice Perfection
Multi-Modal Approach to Healing a Complex Wound: A Case Study Review
Multi-Modal Approach to Healing a Complex Wound: A Case Study Review

Patient
An 84-year-old female was referred with a non-healing surgical wound of the left dorsal foot (Figure 1). She has a history of arterial insufficiency but was deemed a poor candidate for revascularization.
She had been followed by podiatry as an outpatient for several weeks and was taken to the operating room for surgical debridement. Postoperatively I was consulted to assist with limb salvage and specifically coverage of the exposed tendons.
Co-morbidities
In addition to her diabetes, past medical history included hypertension.
Course of Treatment
While awaiting outpatient consultation she was admitted urgently for worsening tissue necrosis and acute infection of the foot. The patient was started on IV antibiotics and immediately on 3M™ Veraflo™ Therapy initiated with 3M™ Veraflo™ Cleanse Choice Complete™ Dressing. After just 1 dressing change there was immediate improvement noted as the necrotic debris was loosened and there was early granulation tissue appreciated (Figure 2).
After the second dressing change, she was taken to the operating room for a surgical debridement (Figure 3). The areas of non-viable tendon were removed, and bleeding tissue was obtained. She was continued on Veraflo Cleanse Choice Complete Dressing for continued wound bed preparation.
While in the acute hospital setting Infectious Disease Specialists provided culture driven antibiotic therapy and the patient’s other medical conditions were managed by the hospitalist. After an additional 72 hours of negative pressure wound therapy with instillation and dwell (NPWTd-i), the patient was returned to the operating room. At this time the wound was clean without necrotic debris. The acute infection was resolved, and the tendon was covered with a placental allograft and reticular dermal matrix as a scaffolding to then allow for definitive skin coverage at a later date. The dermal matrix was dressed with a single layer of 3M™ Adaptic™ Non-Adhering Dressing (Figure 4).

The patient was discharged on oral antibiotics, offloading, and a 3M™ ActiV.A.C.™ Therapy System to continue negative pressure wound therapy (NPWT) with weekly dressing changes. On the first post-operative visit, the patient’s surgical wound was notable for graft adherence. Over the next 5 weeks, the graft fully incorporated (Figures 5-8).
After 6 weeks, the patient was returned to the operating room for definitive coverage with a split thickness skin graft was placed and a single layer of Adaptic Dressing and NPWT with ActiV.A.C. Therapy System. The donor site was dressed with 3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver. The patient was discharged from the hospital and after 7 days of therapy, the NPWT dressing was removed, and skin graft was adherent (Figure 9).
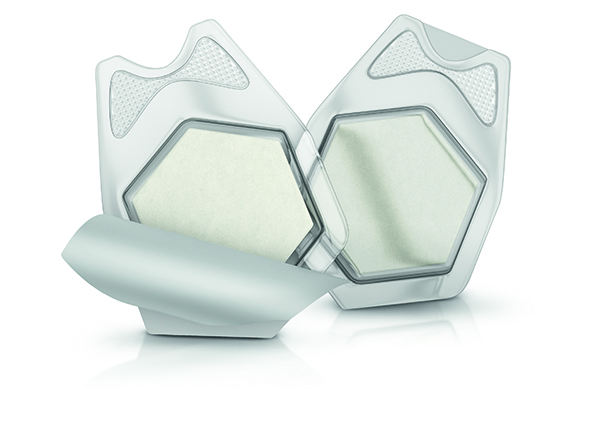
3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver
The patient’s remaining course had been complicated. Post skin grafting, she had a traumatic fall and developed acute ischemia of the foot requiring additional surgery including Transmetatarsal Amputation (TMA) with the need for continued local wound care and NPWT with ActiV.A.C. Therapy System.
The use of the Veraflo Cleanse Choice Complete Dressing accomplished 3 things:
- Easier placement with a combined kit that could be performed in the surgical ward.
- Active therapy to loosen necrotic debris which reduced the need for the operating room and general anesthesia.
- Maintenance of skin integrity with the inclusion of the 3M™ Dermatac™ Drape to protect the peri wound.
Treatment Modalities
- Multidisciplinary team approach
- IV Antibiotic Therapy
- 3M™ Veraflo™ Cleanse Choice Complete™ Dressing
- 3M™ V.A.C.® Ulta Therapy Unit
- 3M™ Dermatac™ Drape
- Operative Debridement
- Placement Reticular Dermal Matrix as Scaffolding
- 3M™ ActiV.A.C.™ Therapy System
- Split Thickness Skin Graft
- 3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver (Donor site)
- 3M™ Adaptic™ Non-Adhering Dressing

(Figure 1) Foot ulcer with tendon exposed.

(Figure 2) 1st Dressing Change.

(Figure 3) 2nd Dressing Change.

(Figure 4) Placental allograft and reticular dermal matrix applied.

(Figure 5) First post-operative visit.

(Figure 6) 2nd week after first post-operative visit.

(Figure 7) 4th week after first post-operative visit.

(Figure 8) Reticular dermal matrix fully incorporated.

(Figure 9) Split thickness skin graft (STSG) adherent.
Conclusion
Non-healing wounds of the lower extremity are common. Limb salvage can be challenging, especially in patients with known arterial insufficiency. Although the probability of amputation is high, reducing the level of amputation to a TMA is beneficial for overall mobility, morbidity, and mortality.
The 3M portfolio is a complete toolbox to assist in the care of these challenging patients. Specifically, the use of the Veraflo Cleanse Choice Complete Dressing may help to actively manage debris while awaiting surgical intervention reducing the need for operative debridement and/or anesthesia. This allowed for subsequent treatment modalities along the wound healing journey such as the ActiV.A.C. Therapy System, Dermatac Drape, and Promogran Prisma Matrix (at the Donor site).
*in-vitro
Do you have questions regarding this case study?
Connect with a 3M Account Representative
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications, warnings, precautions, and safety information exist for these products and therapies. Please consult a clinician and production instructions for use prior to application. Rx only.
Patient data and photos courtesy of Michael N. Desvigne MD, FACS, CWS, FACCWS
Payment for Dr. Desvigne’s services is paid for directly by Present eLearning
To receive information and solutions from 3M subscribe here.
© 2023 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited.

Comments
There are 0 comments for this article