
Practice Perfect 853
It’s In the Blood:
An Anemia Update for the Podiatrist
It’s In the Blood:
An Anemia Update for the Podiatrist
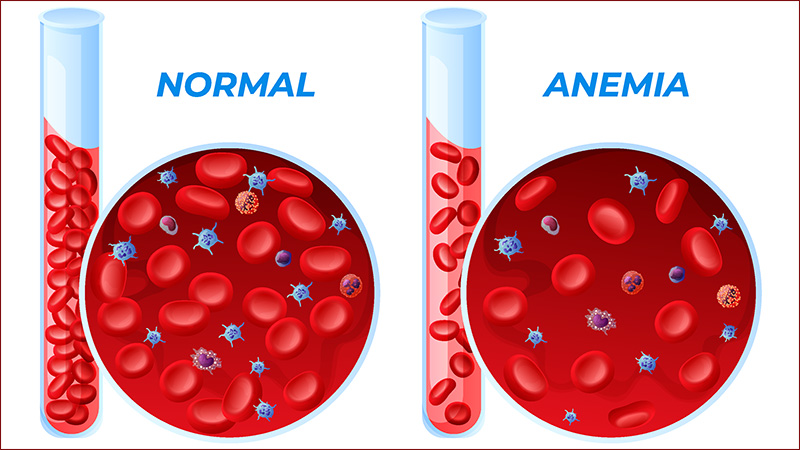
The average podiatrist does not spend a huge amount of time focused on General Medical problems such as anemia. However, as physicians with an emphasis on the lower extremity, we cannot forget the adage, “there is a patient attached to the foot.” As such, it behooves us to maintain our general knowledge of the disorders that might affect our patients. To that end, let's do a quick, high-yield review of anemia.
First, anemia is diagnosed when the hemoglobin level is two standard deviations below the normal for that lab. In general, though, the following numbers tend to be used.
Hemoglobin levels diagnostic of anemia:
Males < 13.5 grams/deciliter
Females < 12 grams/deciliter
Next, we should consider certain situations in which the hemoglobin level might be higher or lower than normal but not necessarily diagnostic of anemia.
Higher Than Normal
- Smoking
- Increased altitude
- Chronic obstructive pulmonary disease
- Right to left cardiac shunts
Lower Than Normal
- African descent
- Pregnancy
- Endurance athletes
- Elderly
It is also important to consider that the presence and severity of patient symptoms depend on the absolute hemoglobin value, speed of development, and comorbidities. It is very easy to misinterpret a low hemoglobin value as clinically significant in a patient with no obvious symptoms. I recently experienced an example of this. I was caring for a 45-year-old type 1 diabetic female patient who had a preoperative hemoglobin of 6.6 g/dL. She was completely asymptomatic and, although the floor nurses were concerned, neither the anesthesiologist nor I were ready to postpone her incision and drainage procedure. The reason for this is that her anemia of chronic inflammation had been a long term, developing problem resulting from her chronic renal disease for which her body had compensated. Now, she did receive a blood transfusion, as will be discussed below, but she remained stable for surgery without complications despite the low hemoglobin.
The diagnosis and treatment of various anemias is beyond the purview of this article, but it is helpful to get a feel for a diagnostic schema to better understand where the medicine team might be heading as we consult on these patients with anemias.
There are two primary approaches to diagnosing anemias, the morphologic approach, which relies on the mean corpuscular volume (MCV), and the kinetic approach, depending on the number of reticulocytes. The latter of these two methods is a little less clinically relevant than the former, so let's talk about the morphologic approach.
Recall that the MCV is found on the complete blood count panel, and the normal is 80-96 femtoliters (fL). Examine the chart below to determine the primary differentials of anemia based off of the MCV.
| MCV < 80 fL = Microcytic | MCV 80-96 fL = Normocytic | MCV > 96 fL = Macrocytic |
|
|
Megaloblastic
Nonmegaloblastic
|
Since it remains commonly used in the hospital, we will also mention reticulocytes. Recall that these are formed in the bone marrow because of the need for more red blood cells. As a result, hypoproliferative anemias result from disorders that do not allow the bone marrow to make more blood cells. This would include nutrient deficiencies, hormone deficiencies, bone marrow failures, anemia of chronic inflammation, and hospital acquired anemia. On the other hand, hyperproliferative anemias occur when the bone marrow is creating a large amount of new blood cells, or reticulocytes. This will usually include blood loss and hemolytic disorders.
This designation is commonly described from the reticulocyte index, which is a somewhat difficult calculation, but some experts are now recommending using the absolute reticulocyte count instead of the reticulocyte index. This is calculated by simply multiplying the red blood cell count by the reticulocyte percent. Remember that the reticulocyte percent must be ordered separately from other blood tests and is not included in an anemia panel.
One cannot help but to discuss blood transfusions in light of the above conversation. Obviously, a podiatrist is not going to order blood transfusions as this should be administered through the medicine team. However, we must keep up to date to have a reasonable conversation with our colleagues when needed.
Blood is most commonly transfused as packed red blood cells or PRBCs. One unit of PRBCs contains 200 mL of red blood cells, 100 mL of an additive, and 30 mL of plasma with a hematocrit approximately 55%. One unit of PRBCs will raise the hemoglobin by 1 g/dL.
In the past, it was common practice to give patients blood when their hemoglobin went below 10 g/dL. The American Association of Blood Banks now recommends instead a strict < 7 g/dL threshold to transfer in patients who are hemodynamically stable1. They firmly recommend, though, that the clinical context should be considered at all times. As mentioned above, my patient was hemodynamically stable, completely asymptomatic, and safe for surgery at a hemoglobin of 6.6 g/dL.
There are so many more aspects of this to explore, and for those who are interested, consider reading the pertinent Up To Date sections or you may consider the YouTube channel Strong Medicine, which is hosted by Dr Eric Strong, a physician from Stanford University. These, and other excellent resources are available for anyone interested. Enjoy your explorations for better patient care in the future.
Best wishes.

Jarrod Shapiro, DPM
PRESENT Practice Perfect Editor
[email protected]

-
Carson JL, Guyatt G, Heddle NM, Grossman BJ, Cohn CS, Fung MK, Gernsheimer T, Holcomb JB, Kaplan LJ, Katz LM, Peterson N. Clinical Practice Guidelines From the AABB: Red Blood Cell Transfusion Thresholds and Storage. JAMA. 2016 Nov 15;316(19):2025-2035.
Follow this link





























Comments
There are 0 comments for this article