
Paths to Practice Perfection
Case Study - Diabetic Foot Abscess and Sepsis: Amputation or Limb Salvage?
Case Study - Diabetic Foot Abscess and Sepsis: Amputation or Limb Salvage?
Patient
A 48-year-old Type II insulin dependent diabetic male presented in the acute care setting with sepsis due to an abscess of the right foot involving bone and deep soft tissue structures of the midfoot. The wound and associated sepsis made limb loss and/or mortality a pressing concern. Options were primary limb amputation versus an attempt at limb salvage.
Co-morbidities
In addition to his diabetes, past medical history included chronic kidney disease stage 3, sleep apnea with continuous positive airway pressure dependence, peripheral neuropathy, hyperlipidemia, hypertension, hypothyroid, morbid obesity, Moya disease, and secondary renal hyperparathyroidism.
Initial Treatment
Incision and drainage of the foot was performed on Day 1 of admission including removal of infected soft tissue and bone, collection of deep tissue cultures, and insertion of calcium sulfate / vancomycin beads in a “bead pouch” technique. The post-debridement defect size was 12cm2. (Figure 1, shows antibiotic bead pouch intact).

Patient was started on a 6-week course of culture-guided IV antibiotics via PICC line and discharged to a skilled nursing unit with instructions to remain strictly non-weightbearing.
On post-operative Day 16 the patient was seen in the outpatient setting and had sharp debridement of the wound and removal of the antibiotic beads. The wound was packed with sterile ¼” gauze packing. He was continued on intravenous antibiotic. He was ordered to remain strictly non-weightbearing. The wound defect size at this point was 13.8cm2 (Figure 2, an overall enlargement from baseline due to sharp debridement) with heavy drainage noted.

Figure 2: Post-Extraction

Figure 3: Extracted Antibiotic Beads
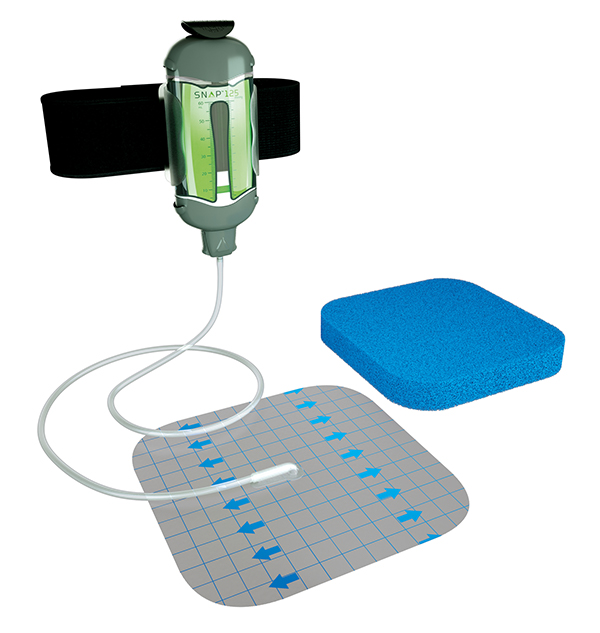
A V.A.C. FREEDOM™ Therapy Unit was ordered to be placed on post-operative Day 17 while in the skilled nursing facility and changed three times per week with 3M™ V.A.C.® Granufoam™ Dressings at 125mmHg negative pressure.

The patient was seen on post-operative Day 37 as an outpatient, and the wound measurement was noted to be 7.5cm2 (Figure 5, 45.65% reduction in area from post-operative Day 16 measurement) with light drainage (less than 180ml per week). Sharp debridement was performed (Figure 6).

Figure 5: Pre-Debridement

Figure 6: Post-Debridement Which Increased Wound Defect Size
V.A.C. FREEDOM™ Therapy System was reapplied and ordered to be changed three times a week. Strict non-weightbearing encouraged. He was prepared to return to the home setting once his full course of intravenous antibiotics was complete. The patient was seen on post-operative Day 51 in the office setting and the wound measurement was noted to be 10cm2 (27.54% reduction in area from post-operative Day 16 measurement).
An order was placed for a home health care agency to place a 3M™ Snap™ Therapy System at 125mmHg continuous negative pressure with 3M™ Snap™ Advanced Dressing Kit (Figure 7) twice per week on the wound once he was in the home setting. Intravenous antibiotics were completed. Sharp debridement was performed. Orders were given to continue Snap Therapy System with home health care services and remain non-weightbearing.

Figure 7: 3M™ Snap™ Advanced Dressing in Place

Figure 8: 3M™ Snap™ Therapy System in Place
The patient was seen on post-operative Day 65 in the office setting. Sharp debridement performed. Order given to continue Snap Therapy and non-weightbearing. Wound measurement 6.75cm2 (Figure 9).

The patient was seen on post-operative Day 86 in the office setting. Sharp debridement performed. Order given to continue Snap Therapy System and non-weightbearing. Wound measurement 3.6cm2 (Figure 10).

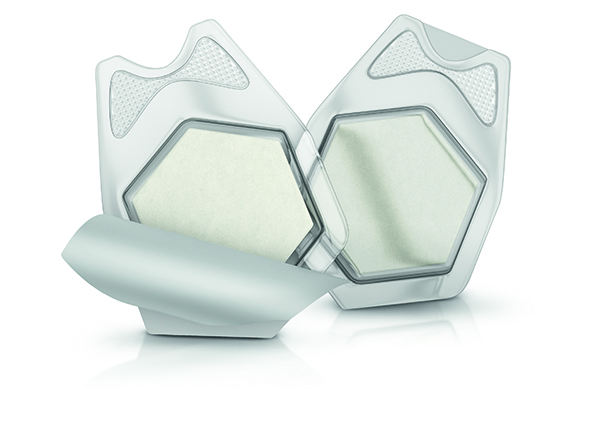
The patient was seen on post-operative Day 107 in the office setting. Sharp debridement performed. Order given to discontinue Snap Therapy and transition to 3M™ Promogran Prisma™ Matrix (Figure 11) three times per week. Patient instructed to begin guarded weightbearing in a removeable cast boot. Wound measurement 1.8cm2 (Figure 12).

Figure 11: 3M™ Promogran Prisma™ Matrix

Figure 12: 86.96% reduction in area from post-operative Day 16 measurement
The patient was seen on post-operative Day 123 in office setting where wound closure and complete healing were noted (Figure 13). Wound care orders discontinued. Patient instructed to transition back to his normal diabetic footwear.

Treatment Modalities:
- Antibiotic beads
- Sharp debridement
- IV antibiotic therapy
- V.A.C.® FREEDOM™ Therapy Unit
- Removable cast boot
- 3M™ Promogran Prisma™ Matrix
Conclusion
The wound resulting from the infection and subsequent incision and drainage penetrated almost from dorsal to plantar foot and involved skin structures, deep soft tissue structures (ligament and tendon) as well as bone. An amputation was avoided in this case through the combination of an aggressive series of sharp debridements, a period of non-weightbearing and the use of NPWT. Following discontinuation of NPWT, collagen + silver oxidized regenerated cellulose was applied to wound for 16 days with complete healing noted on Day 123.
Do you have questions regarding this case study?
Connect with a 3M Account Representative to learn more.
Patient data and photos courtesy of Brent Bernstein, DPM.
Note: Dr. Bernstein was a paid consultant for KCI products at the time of this case study.
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications, warnings, precautions, and safety information exist for these products and therapies. Please consult a clinician and production instructions for use prior to application. Rx only.
© 2021 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited. PRA-PM-US-03488 (06/21).

Comments
There are 2 comments for this article
Very nice case! Only thing to add is due diligence for vascular patency.
Excellent case. I was wondering if you could have performed a plastic closure 2 weeks after the VAC was applied.